Heart disease is the No. 1 killer in America, outpacing cancer just slightly. The mechanics are simple. It fails to pump blood through the human body due to either blockage of the feeder arteries and the heart muscle starved of oxygen rich blood dies. The the heart stops, and then you die.
But what if surgeons could replace the heart with a durable and permanent replacement device that could pump blood reliably without the need for replacement for a long long time – longer than the natural lifespan of a human (which is typically around 79 years in the U.S.).
In the book Super You, we reported that a device like that would save 614,348 American lives each year (based of 2105 CDC data) and millions more worldwide.
Up until now, there’s been no artificial heart candidate that can be a permanent replacement for the biological pump humans are born with. There have been some noble efforts, however most of the devices act as bridge technology that can keep a heart patient alive until a transplant organ becomes available.
The human heart is a very efficient pump, and tough to replace with a mechanical device. There’s not much space in the chest cavity. There are issues of durability. It needs to operate efficiently for 80 years or so and increasingly longer. And it needs to be powered.
We discovered as we researched our book, that in the next two years or likely sooner thereafter, that is likely to change.
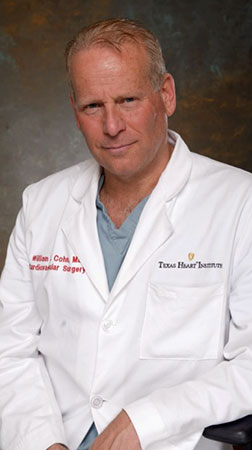
In the book Super You: How Technology is Revolutionizing What it Means to Be Human my co-authors and I interviewed Dr. Billy Cohn, who along with his partner Dr Bud Frazier, have developed a heart-assist device which is used commonly used to help an ailing human heart push blood. Cohn and Frazier are researchers at the Texas Heart Institute in Houston,
The two doctors have since partnered with Dr Daniel Timms, an Australian inventor, whose father died of congestive heart failure. Timms was driven to invent a permanent heart replacement device. However he ran out of funding and resources, but reached out to Cohn and Frazier, and his design along with their expertise, support and funding have filled in the shortcomings of the Texas-designed device and now it’s almost ready for human primetime transplant.
But first some background…
In the 1980s, physician inventor Rich Wampler visited Egypt and witnessed local workers using a hand-turned Archimedes screw to pump water up a river bank for irrigation. (See video of the screw: Video: The Archimedes Screw.)
He realized that if a screw could move water against gravity, perhaps it could move blood against pressure. So he designed a prototype that used an external motor outside the body to spin a small screw the size of a pencil eraser 25,000 times per minute inside the body.
Perhaps, he reasoned, it could pull a meaningful amount of blood out of a weakened ventricle to get a patient through a short period of heart failure.
Wampler showed the device to Frazier, who was initially concerned that the rapidly spinning screw would destroy fragile blood cells. Research showed it wasn’t an issue, so, in 1988, the device was used to help save a dying patient. A number of durable, permanent, screw-like assist pumps were developed over the next few years. Unlike the assist pumps that beat like the human heart, these rapidly spinning pumps were much smaller and much more durable.
“These continuous flow pumps have no flexible membranes, no cams, no cam followers, no high torque rotors,” said Cohn. “The new pumps eliminate all that mechanical complexity … they’re small, they’re quiet, and they’re very durable.”
In these earliest heart-assisting devices, the spinning screw, sometimes also called an “impeller,” was supported with a mechanical bearing that was impervious to wear and was kept clean by the rapid flow of blood.
“There was one moving part, so nothing to fail,” Cohn explained.
With the newest generation of assist pump, the spinning impeller is suspended in a magnetic field. Now, even the bearings have been eliminated.
Enter the jet-engine heart.
One of the first of these spinning assist pumps was the HeartMate II, a device that assists a weakened heart by drawing blood from the left ventricle.
It is just like the one Vice President Dick Cheney had implanted.
Now, many heart centers have tried to implant a pair of assist pumps; one in each ventricle…but it is not ideal because two controllers are needed and there is limited space inside the chest. Cohn and Frazier began to investigate if it would be possible to remove the heart completely and replace it with two spinning pumps.
Although a significant percentage of patients implanted with continuous flow assist pumps lose their pulse, the pressure in the arteries still rises and falls with each heartbeat—just not enough to be felt with fingertips.
Cohn and Frazier’s idea was validated through extensive research in the large animal facility at the Texas Heart institute. It showed conclusively that calves could be kept alive with continuous flow devices. The animals would eat, sleep, and grow like normal calves, and would interact with caregivers and exercise on a treadmill, and yet they had no heartbeat, no EKG, and no pulse.
In 2011 a gravely ill man, arrived at the Texas Heart Institute. His diseased heart was replaced with a pair of HeartMate II pumps. The device kept Lewis alive for more than five weeks, and it even allowed him to sit up and interact with his family after a prolonged pre-operative period. Lewis died from progressive failure of some of his other organs. But, the heart replacement showed it was possible to live without the original organ for longer periods.
Through all this work, Cohn and Frazier talked about their research at professional society meetings and at speaking engagements. It included a talk at TEDMED in 2012.
As a result of that exposure, they met Daniel Timms, an Australian scientist living in Australia.
He independently came upon the idea that a continuous-flow device was the way to go. His unique design addressed many of the challenges caused by a pair of spinning pumps. And it wasn’t unlike the technology being used by Frazier and Cohn.
The device Timms created contained a single moving part suspended in an electromagnetic field. The single spinning disc had impeller vanes on each of the two faces. One side took the bright red blood returning from the lungs and pumped it to the rest of the body. On the other side of the same spinning disk, vanes drive the blood returning from the body to the lungs. The one spinning disk performs the function of two pumps.
Timms designed the spinning disc to shift slightly from one side to the other, based on changes in pressure. This resulted in a change in the relative strength and efficiency of the left and right pumps. It responds to physiological changes faster than a natural human
heart. The strength of the electromagnetic field is adjusted 20,000 times each second to keep the disc spinning in space.
Timms didn’t have the resources, institutional experience, and support to get the device to work. But when he happened on the Cohn-Frazier TEDMED talk, he flew to the Houston.
“He was unshaven, and had on blue jeans, but he seemed like a nice young man, so I was going to let him down softly when I figured out why his device was tragically flawed, as soon as I figured it out,” Cohn told us in an interview for the book, recounting the meeting.
But Timms’ pitch was brilliant. “He starts describing this device. I sort of cross examine him. I say ‘What about this? What about that?’ He had great responses to everything,” said Cohn. “We had scheduled a 30-minute meeting. And after talking to him for three hours, I realize this guy is one of the most brilliant men I’ve ever met, and his device addresses many of the challenges and shortcomings of our twin turbine concept.”
 Specifically, it had the potential to be much smaller. It automatically balanced the left and right sides of the circulation. It would only require a single controller. And, most importantly, it wouldn’t wear out after a year.
Specifically, it had the potential to be much smaller. It automatically balanced the left and right sides of the circulation. It would only require a single controller. And, most importantly, it wouldn’t wear out after a year.
Cohn and Frazier invited Timms and his team to come to Houston. To back Timms, the Texas Heart Institute team leveraged their expertise, network, and their ability to raise money, and used their experience with heart replacement and their large animal lab to move the project forward. Dr. Frazier and Dr. Cohn persuaded gifted engineer, Dr. Daniel Timms, and his team to relocate from Australia and Germany to the Texas Heart Institute in Houston to work on their BiVACOR total artificial heart device
The results to date have been extremely encouraging, so much so that Frazier and Cohn are fairly convinced that the device will be the first practical permanent mechanical replacement for the failing human heart.
By the way, the device will be powered by a short-range wireless power transmitter that uses external batteries that generate a high-intensity oscillating magnetic field. It is beamed into the body to power the heart-replacement device in the chest.
You can read this story in greater detail in Super You – get it from Amazon. Or order Super You online directly from Pearson, our publisher (ebook or paperback).
For a free sample chapter – focusing on hyper longevity, CLICK HERE